Peyronie's Disease

WHAT CAUSES PEYRONIE’S DISEASE?

The ExoSurge® "Working Theory" Model
You can't solve a problem until you know what it is.
How could we develop a long-term solution for Peyronie's disease if we didn't know what's causing it in the first place? That was something we didn't believe was possible. We also believed this was the reason all treatments to date fell short: they all focused on treating specific Peyronie's symptoms rather than addressing the disease's root cause.
We considered it critical to build working ideas surrounding the origin of Peyronie's Disease over our twenty-year journey creating innovative technologies that permanently remove the fibrosis and penile plaques that cause a Peyronie's diagnosis.
Those working theories were a moving target early on, but when our technology proved effective, they became more static over the last seven years.
Our working hypothesis for Peyronie's Disease causation is complex and incorporates case and patient-specific characteristics. To improve clinical accuracy, more research will be needed in the future.
However, using our working theory method in conjunction with our therapy devices and protocols, we've reached a stage where all, or 100%, of Peyronie's patients who finish treatment with our technology see a permanent reduction in penile fibrosis and plaques.
What Causes Peyronie’s Disease?
We believe Peyronie’s disease is triggered from a wide variety of potential sources of penile trauma[1]. We have discovered the existence of what we call “Peyronie’s Accelerators” that can cause a benign case to evolve into a problematic Peyronie’s diagnosis. Finally, select “predisposed” patients are much more prone to build up fibrosis equating to a Peyronie’s diagnosis even after only a singular microtrauma.
Penile trauma[2] has long been suspected as the source of Peyronie’s from studies[i]. However, there remained cases that could not be explained where the patient had no recollection of any penile injury.
Based upon distinct variations in the design and the thickness of treated Peyronie’s plaque combined with an analysis of patient history, we were able to differentiate dissimilarities in the penile fibrosis and categorize them into varied degrees of trauma plus classifiable time spans since the plaque is measurably unique in design and density for those instances.
Additionally, there’s a select group of Peyronie’s accelerators that can trigger rapid onset of Peyronie’s plaque or engender a stable case to become problematic after years or decades of undetectability.
[1] Zargooshi J. Trauma as the cause of Peyronie's disease: Penile fracture as a model of trauma. J Urol 2004;172:186-8.
[2] The pathophysiology of Peyronie's disease: beyond the Smith's space
Int Braz J Urol, 41 (2015), pp. 1040-1042.
We believe Peyronie’s disease is triggered from a wide variety of potential sources of penile trauma[1]. We have discovered the existence of what we call “Peyronie’s Accelerators” that can cause a benign case to evolve into a problematic Peyronie’s diagnosis. Finally, select “predisposed” patients are much more prone to build up fibrosis equating to a Peyronie’s diagnosis even after only a singular microtrauma.
Penile trauma[2] has long been suspected as the source of Peyronie’s from studies[i]. However, there remained cases that could not be explained where the patient had no recollection of any penile injury.
Based upon distinct variations in the design and the thickness of treated Peyronie’s plaque combined with an analysis of patient history, we were able to differentiate dissimilarities in the penile fibrosis and categorize them into varied degrees of trauma plus classifiable time spans since the plaque is measurably unique in design and density for those instances.
Additionally, there’s a select group of Peyronie’s accelerators that can trigger rapid onset of Peyronie’s plaque or engender a stable case to become problematic after years or decades of undetectability.
[1] Zargooshi J. Trauma as the cause of Peyronie's disease: Penile fracture as a model of trauma. J Urol 2004;172:186-8.
[2] The pathophysiology of Peyronie's disease: beyond the Smith's space
Int Braz J Urol, 41 (2015), pp. 1040-1042.
Observations: Peyronie's Accelerators
How is it that a man awakens and notices his morning erection is now noticeably curved when it was perfectly straight the night before?
This common starting point for a Peyronie's diagnosis remained one of the biggest stumbling blocks with almost every explanation for the epidemiology behind Peyronie's disease.
Peyronie's Accelerators, conditions that can trigger a long benign case of fibrosis to quickly grow larger and cause noticeable Peyronie's symptoms were an important discovery from our years of research.
We unearthed six unique Peyronie's Accelerators that will cause a patient with an unrecognized history of perpetual microtrauma to immediately experience notable Peyronie's symptoms regardless of general health.
Our research shows patients sometimes require two Peyronie's accelerators before symptoms become significantly noticeable.
While we have identified six accelerators, we continue to seek anymore from cases where treatment is more challenging than usual.
Peyronie's Accelerators have a substantial effect on treatment efficacy.
As their name suggests, Peyronie's Accelerators exacerbate a PD case. Peyronie's accelerators make it more difficult to achieve measurable penile plaque reduction, even with ExoSurge® technology, when left untreated. The good news is that all accelerators can be treated clinically, and we have identified the quantitative metrics at which these conditions need to be to achieve optimal results. Plaque reduction improvement, however, can be particularly difficult to improve if a patient does not follow prescribed instructions regarding management of accelerators.
Peyronie's Accelerators have likely skewed Peyronie's clinical studies results for decades
Clinical studies for new types of Peyronie's care are an additional important issue concerning Peyronie's Accelerators.
These six accelerators are nearly on par with the size and density of fibrous tissue plaques in terms of their impact on quantitative improvement. In other words, based on our findings in this regard, many historical comparative studies of Peyronie's disease treatments were inherently fraught with erroneous results from the beginning, as no one accounted for the existence and management of these accelerators in patient selection, treatment, or outcome comparisons.
After all of our patents have been filed, we will divulge information regarding the identification, treatment, and management of Peyronie's Accelerators.
Observations: There is no "lucky" 13%
The current standard of care for PD recommends a "hands-off" approach to the active phase of Peyronie's disease because "13% of Peyronie's cases go away on their own." These patients have sometimes been referred to as the lucky 13%.
How many patients men have heard, "In some cases, Peyronie's disappears on its own after the initial onset"? As a foundational tenet of our therapeutic approach, we shared this common belief for years.
We now have serious doubts about this supposition. In other words, we believe certain healthy males can temporarily overcome the symptoms of a Peyronie's disease diagnosis following an acute penile injury. Nonetheless, once one or more Peyronie's accelerators eventually take effect? These same patients will experience Peyronie's disease symptoms from the original injury.
Three patients under our care who had previously sustained a penile injury recalled having palpable fibrosis and erect penile curvature, and the condition resolved on its own. In light of diminishing health inputs, let's fast forward twenty years. Return of the curvature and perceptible firmness. In the absence of urologist-performed duplex Doppler imaging of the area where the plaque "disappeared," we can only speculate as to whether this is the case.
We believe it is possible for some men with acute penile fibrosis to self-improve. (We're getting close to accurately identifying the health and genetic markers of those men).
Nonetheless, if Peyronie's disease is caused by perpetual microtrauma and Peyronie's Accelerators? There is no possibility that the patient will self-improve.
Observations: Genetic Susceptibility for Peyronie's Disease
A patient with select genetic “predisposition for Peyronie’s” factors will almost always eventually end up with a PD diagnosis. Such predispositions transform what would be an asymptomatic micro trauma for an unaffected male into a full-fledged Peyronie's case with heavy fibrotic plaque response for the genetically predisposed patient.
We sometimes liken this condition to that of a hemophiliac. With significant hereditary predisposition, even regular sexual intercourse and manual masturbation is sometimes enough to trigger the disease in these men.
Men with a congenital curvature (Chordee) can be classified as a subset of predisposition for Peyronie’s, although they can’t acquire it nearly as easily as men with select hereditary conditions.
However, we believe the likelihood of injury during sexual intercourse for patients with Chordee is about double that of a male without a congenital curve.
Observations: Acquired Predisposition for Peyronie’s Disease
One of the most common Peyronie's Accelerators we discovered is identified from blood testing and often successfully treated with medications.
We believe that this "acquired predisposition" for Peyronie's disease is a major contributor to the 900% increase in Peyronie's prevalence among men aged 18 to 24 in the United States.
Management of this issue is key to treatment success with plaque removal and will likely be an important building block for Peyronies prevention in the years ahead.

Observations: There are at least 10 Variations in Peyronie’s Penile Plaque
Historically, Peyronie's plaque was classified in one of two categories: calcified or non-calcified.
Our research uncovered ten distinct types of penile fibrosis and plaques associated with Peyronie's disease. Each requires a modified approach to penile plaque removal. It is important to note that in many instances, a patient will have more than one of these major forms of plaque simultaneously.
After completing our intellectual property filings, we will publish information about these unique Peyronie's plaque variations and the optimal treatment for each.
It is one of the most exciting aspects of our Peyronie's disease epidemiology discoveries.
Observations: Variations in Penile Trauma That Trigger Peyronie’s
Following are what we consider to be the most common sources of penile trauma that trigger a Peyronies indication based upon review of our patient treatment histories.
Also, we share information about certain “Peyronie’s Accelerators” – conditions which can cause a full Peyronie’s diagnosis to occur more quickly or more severely.
Finally, there’s a list of circumstances where a patient is “predisposed” to get Peyronie’s through only slight microtrauma. We equate “predisposition” patients as “hemophiliacs” of Peyronie’s.
Finally, it’s worth noting that we encountered cases where these varied trauma categories occurred in tandem to one another. For instance, a patient could have some long-established penile plaque from perpetual microtraumas that’s not yet outwardly exhibiting Peyronie’s symptoms and then subsequently incur a direct penile injury which triggered a significant Peyronie’s indication. This means the complete picture of penile plaque in such a case must be addressed differently because of the variations in related plaque shape and density.
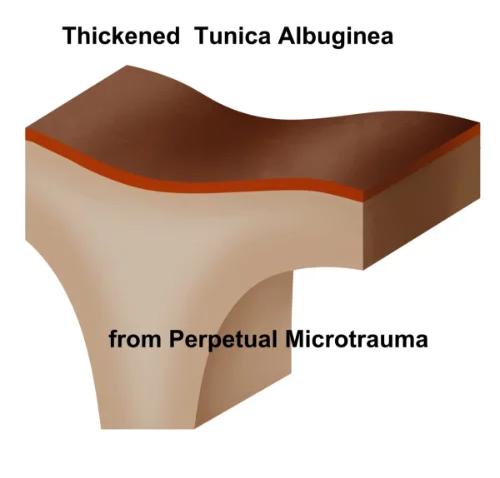
1. Perpetual Penile Microtrauma
The most common source for fibrotic plaque that triggers a Peyronie’s indication occurs from years of microtraumas[1] to the penis. According to studies, about 75% of Peyronie’s cases are derived from patients with no clear recollection of any specific trauma.

In some instances, we found that perpetual penile microtrauma seemed to evolve into a full-fledged Peyronie’s diagnosis from “the feather principal” – where just one additional minor penile trauma tips the scales into an easily verified Peyronie’s diagnosis. However, most commonly the evolution from a benign case to visible symptoms is triggered by Peyronie's Accelerators.
What we noticed is that Peyronie's plaque that’s derived from a long term run of penile microtraumas most commonly resembles one of two designs:
1. Interwoven spiderweb within the penis tissue.
2. Thickened Tunica

We theorized the initial microtrauma(s) triggered a fibrotic response to the penis. In time, as the body senses “something is still wrong” in that area of the penis, the body sends additional fibrotic material to heal what was unresolved after the first minor trauma. That additionally generated fibrotic material rarely ends up in exactly same spot as the first indication. Rather, most often it ends up very nearby. Hence the spider web and woven nature of this penile plaque. We believe those cases of similar patient history where the Peyronie’s indication is primarily rooted in a thickened tunica are likewise slow and perpetual in growth based upon variations we encounter with Tunica density. Tunica thickening can manifest from both its size and density.

We further postulated that many younger and healthy patients could naturally keep continued growth of fibrosis minimized. However, as that same patient ages[2] and their health dynamics decline, a Peyronie’s indication becomes inevitable.
The exact sources for these penile microtraumas are as diverse as the human experience. It was the variations in the density and design of the microtrauma-based plaque combined with patient interviews that we were able to ascertain this key origin of Peyronie’s disease. The variations in density of plaque amongst the spiderweb like plaque striations offers a tell-tale signal that some of these microtraumas could go all the way back to “missed ground balls” from Peewee baseball to grinding against a female partner’s pelvic bone for hours during teen years intimate exploration.
Sometimes the tipping point for a Peyronie’s indication from perpetual microtrauma isn’t derived from an additional trauma but rather, the introduction of one or more of the Peyronie’s accelerators. We have discovered six unique Peyronie's accelerators which will be share soon in our published study. These accelerators disrupt the body’s mechanisms to keep the growth of fibrosis at bay which often triggers a Peyronie’s case to go from unnoticeable to hindering sexual fulfillment from seemingly “thin air”.

These latter elements support the logic behind Peyronie’s being most common within older patients as they’ve had a lifetime to endure a buildup of penile microtraumas and are the most susceptible to ending up with a Peyronie’s accelerator from their older health paradigm and decline of well-being from aging or diseases from compromised health.
Most commonly, we encounter a combined tandem of fibrosis, plaques, and tunica thickening during evaluation, with the size and degree of problem from each varying by case.
Tunica thickening, without any fibrosis or plaques is sometimes discovered which is why we added “and/or tunica thickening” to our improved definition of Peyronie’s disease. We hypothesize tunica thickening will be a key aspect for future studies on perpetual penile microtrauma and Peyronie’s Disease in the years ahead.
[1] De Rose, Aldo, Mantica, et al, Supporting the role of penile trauma and micro-trauma in the etiology of Peyronie’s disease. Prospective observational study using the electronic microscope to examine two types of plaques –Pages 740-745 | Received 02 Jan 2019, Accepted 17 Feb 2019, Published online: 16 Mar 2019
[2] Inhibition of histone deacetylase 2 mitigates profibrotic TGF-β1 responses in fibroblasts derived from Peyronie's plaque
Asian J Androl, 15 (2013), pp. 640-645
2. Direct Penile Injury
The second most common source for a Peyronie’s indication comes from meaningful and memorable direct injury to the penis. Certain sexual activity during intercourse are common sources of direct penile injury including injury from a sexual partner being “on top” and coming down at an unagreeable angle upon the penis or overly aggressive thrusting during intercourse which triggers injury from misalignment.

The variety among non-sexual direct penile injury sources is utterly endless: significant impact to the penis from some sort of freak accident, sports injuries to the groin, etc. One of our patients ended up with direct penile injury triggering Peyronie’s after losing his footing while hiking in the Yukon and briefly slipping into freezing waist deep water.
Direct penile injury Peyronie’s plaque manifests in a manner most represented in popular Peyronie’s medical illustrations – it often resembles a kind of a “big glob” of fibrous tissue plaques.
The second most common source for a Peyronie’s indication comes from meaningful and memorable direct injury to the penis. Certain sexual activity during intercourse are common sources of direct penile injury including injury from a sexual partner being “on top” and coming down at an unagreeable angle upon the penis or overly aggressive thrusting during intercourse which triggers injury from misalignment.

The variety among non-sexual direct penile injury sources is utterly endless: significant impact to the penis from some sort of freak accident, sports injuries to the groin, etc. One of our patients ended up with direct penile injury triggering Peyronie’s after losing his footing while hiking in the Yukon and briefly slipping into freezing waist deep water.
Direct penile injury Peyronie’s plaque manifests in a manner most represented in popular Peyronie’s medical illustrations – it often resembles a kind of a “big glob” of fibrous tissue plaques.

3. Healthcare Related Penile Injury
Healthcare related penile injury that triggers PD is damage that occurs during healthcare procedures. Most commonly, this source of PD happens during use of urinary catheter during anesthesia or a therapeutic for bladder control during anesthesia. Occasionally, a nurse will inadvertently inflate a catheter in the urethra versus the bladder: triggering injury. Additionally, some patients are born with an inherently narrow urethra making them more prone to suffer penile injury from catherization. We’ve seen patients suffer Peyronie’s triggering plaque from a catheter installed to protect the penis during certain cancer therapeutics. The second most common healthcare based penile injury occur from a prostatectomy. While a radical prostatectomy often results in worse damage, some patients suffer a fibrotic response from a robotic prostatectomy.
Healthcare related penile injury that triggers PD is damage that occurs during healthcare procedures. Most commonly, this source of PD happens during use of urinary catheter during anesthesia or a therapeutic for bladder control during anesthesia. Occasionally, a nurse will inadvertently inflate a catheter in the urethra versus the bladder: triggering injury. Additionally, some patients are born with an inherently narrow urethra making them more prone to suffer penile injury from catherization. We’ve seen patients suffer Peyronie’s triggering plaque from a catheter installed to protect the penis during certain cancer therapeutics. The second most common healthcare based penile injury occur from a prostatectomy. While a radical prostatectomy often results in worse damage, some patients suffer a fibrotic response from a robotic prostatectomy.
4. PGE Injections
We unearthed a new source of repeated microtrauma that’s been overlooked within urology - needle administration of Alprostadil (PGE) injections for treating erectile dysfunction. While standards of care tout long term use of PGE as relatively safe, we continue to encounter patients suffering from intracorporeal fibrosis triggered by PGE therapy.
After noticing a trend among new patients arriving for Peyronie’s care that was sourced to damage caused from long term use of prostaglandin E1 (for two years or more) in 2018, we began performing duplex Doppler ultrasonography tests on every new ED patient with a history of Tri-Mix injections.
We discovered 61% of patients who had over two years with regular deployment of PGE injections had measurable fibrotic buildup of intracorporeal fibrosis near the injection site areas.
Based upon this observation, we launched a program administering a singular ExoSurge® therapeutic monthly for all new and ongoing patients getting PGE injections. Subsequently, none of our patients receiving PGE injections showed any measurable fibrous tissue plaques.

We unearthed a new source of repeated microtrauma that’s been overlooked within urology - needle administration of Alprostadil (PGE) injections for treating erectile dysfunction. While standards of care tout long term use of PGE as relatively safe, we continue to encounter patients suffering from intracorporeal fibrosis triggered by PGE therapy.
After noticing a trend among new patients arriving for Peyronie’s care that was sourced to damage caused from long term use of prostaglandin E1 (for two years or more) in 2018, we began performing duplex Doppler ultrasonography tests on every new ED patient with a history of Tri-Mix injections.
We discovered 61% of patients who had over two years with regular deployment of PGE injections had measurable fibrotic buildup of intracorporeal fibrosis near the injection site areas.
Based upon this observation, we launched a program administering a singular ExoSurge® therapeutic monthly for all new and ongoing patients getting PGE injections. Subsequently, none of our patients receiving PGE injections showed any measurable fibrous tissue plaques.

5. Millennial Penile Trauma
A rapidly growing new source for a Peyronie’s indication was unearthed from a pair of recently published study regarding Peyronies prevalence by Stuntz, et al[ii]. This study sought to remove much of the embarrassment associated with Peyronie’s in its questionnaire and one even broke down a Peyronie’s indications by demographics such as age, income, and geography.
What “jumped off the page” when examining these numbers was the age group with the highest percentage for Peyronie’s indications: 18-24 year old men. Historically, the percentage of men with any sort of Peyronie's indication was only 1.5%. The Perlacky, et al prevalence study pegged this group at set as 15%, an alarming 900% increase.
Why the huge increase with prevalence of Peyronie's?
No studies have been conducted to determine the cause of this massive increase.
However, researchers at ExoSurge® have discovered a condition that's identified through a simple blood test that every Peyronie's patient we have treated tested positive for. It's included among our list of Peyronie's accelerators. This breakthrough could prove to be crucial with preventative Peyronie's care in the future.

To learn more about our diagnostics and Peyronie's treatments with ExoSurge technology right away, please visit our clinical website and schedule a "one on one" phone consultation or a visit to our clinic in the Buckhead area of Atlanta, Georgia.
Stay Up To Date
If you are a Peyronie's patient who has interest in participating in one of our upcoming clinical trials around the United States, please click here
If you are a urologic clinician who has a potential interest with being involved in our upcoming prospective clinical trials, please click here
If you would like to stay abreast of our progress during clinical trials and in the future, please click here:
Sign up to follow our story and to watch us grow!